Collagen Cross-linking (CXL) is a non-invasive treatment for the thinning and distortion of the cornea that can occur in keratoconus and post-LASIK ectasia. In the CXL procedure, Riboflavin (Vitamin B2) eye drops are instilled into the eye. Next, the cornea is exposed to ultra-violet (UV) light, and the Riboflavin reacts with the UV light, to create new collagen bonds (cross-linking) and thus strengthen the cornea.
By creating new collagen bonds, CXL increases the structural integrity of corneas weakened by keratoconus and ectasia. Cross-linking is a normal function of collagen, and our corneas will naturally cross-link over time, from the UV light to which we are all exposed when we walk outside in the sunlight. (This is one of the theories why the progression of keratoconus seems to slow by age 40 to 50 – the UV light from the environment slowly cross-links our corneas)
CXL accelerates this natural process of the bonding of the layers of the cornea, and increases the natural strength of the cornea without affecting its clarity. When performed early enough, CXL can allow good vision to remain, and prevent further corneal degeneration. In more advanced cases, CXL can stabilize vision, and some people report that their contact lenses are more comfortable and vision is sharper. CXL can also postpone the need for invasive treatments, such as corneal transplantation. We have also seen some cases of improvement in the cornea after CXL.
While not available in the US yet, there is a technology in Europe and Canada that allows for laser vision correction after CXL for patients with keratoconus and ectasia.
What is Keratoconus?
Keratoconus is an inherited condition, in which there are too few collagen bonds in the cornea to maintain structural integrity. Over time, the cornea looses its natural “dome-like” shape and takes on a “cone-like” shape. (Imagine an IKEA bookshelf, in which the pieces are not connected tightly – the furniture starts to tilt and lean.) Many patients with keratoconus also have allergies and “itchy eyes.” We believe that the combination of genetically decreased natural strength of the cornea, and the frequent eye rubbing seen in people with eye allergies, triggers the thinning of the cornea and creates keratoconus.
As the cornea is the clear part of eye responsible for focusing light, this irregular shape causes blurry vision, which can often not be corrected with glasses or soft contact lens. Keratoconus is often progressive, and gets worse over time. Most people with keratoconus notice that their vision is getting worse at age 15 to 20 and they are told that they are becoming more astigmatic. However, in keratoconus, the astigmatism is irregular, meaning that glasses and soft contact lenses will not fix the problem. It is not normal to become more astigmatic every year, and this is often the first sign of keratoconus. Using advanced imaging, called corneal topography, and anterior segment OCT imaging, we can determine if irregular astigmatism due to keratoconus is present, and how severe the condition is.
What is Post-LASIK ectasia?
Post-LASIK ectasia can occur when the cornea begins to thin after laser eye surgery, and vision begins to get very blurry. (While less common, ectasia can occur after any corneal surgery to improve vision, such as PRK or RK.)
What is the difference between “regular” astigmatism and “irregular” astigmatism?
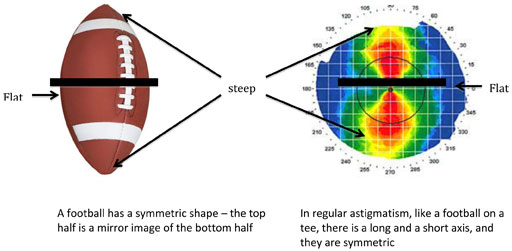
Some people have been told that a cornea with astigmatism is shaped like a football. This is a slight exaggeration, but the point is valid. A cornea with astigmatism is slightly longer in one direction and slightly shorter in another direction. In regular astigmatism, the cornea is more oblong shaped, like a football. A football is symmetric, meaning that you could cut the football in half in the middle and the two halves would be the same shape, in regular astigmatism, the cornea is symmetric.
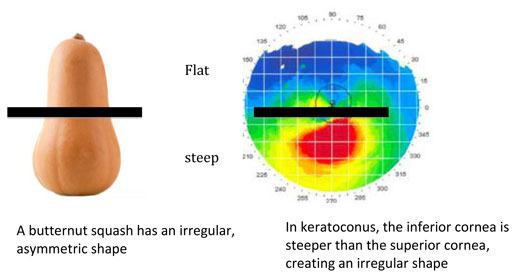
People with irregular astigmatism have a cornea shaped more like a squash, with the inferior portion of the cornea having a “steeper” shape than the top half of the cornea.
Frequently Asked Questions
CXL
In Europe, CXL was approved for widespread use in 2006. The FDA in the US approved CXL in April, 2016.
Dr. Levinson participated in the clinical trials of collagen cross-linking with Avedro, which have led to FDA approval, and has been performing CXL since 2012.
Studies have shown that CXL stops progression of keratoconus in most patients. Some patients will have a subjective increase in vision (objects appear more sharp and crisp), improved contact lens tolerance, and improvement in the shape of the cornea (noted on the computerized topography)
Epithelium-off CXL involves gently removing the layer of skin, called the epithelium that covers the cornea. Then the riboflavin eye drops are placed on the cornea and the cornea is exposed to UV light. We have longer clinical experience with Epi-off CXL, and most studies evaluating the effect of CXL has been with the epi-off technique.
Epithelium-on CXL does not remove the epithelium of the cornea.
Epi-off CXL has the most scientific evidence to support its effect and this is the version that has been performed most frequently world-wide.
Removing the epithelium of the cornea can cause pain and discomfort for 1 week or more. There is also a small risk of infection, and delayed healing of the epithelium. We need to hold off on restarting contact lens use until the epithelium is fully healed. In patients with prior eye surgery, such as LASIK, removing the epithelium carries further risks, as well.
Epithelium-on CXL has minimal discomfort after the procedure, and most people have no discomfort after 12-24 hours. Contact lens use can be restarted after 48-72 hours.
Epithelium-on is a newer technique and there are fewer scientific papers to support long-term results.
The epi-on CXL is performed in our office and the riboflavin eye drops are administered for 60 minutes, and then the cornea is exposed to 10 minutes of UV light. Then a contact lens is placed on the eye for comfort.
The epi-on CXL is performed in the procedure room at the hospital and the riboflavin eye drops are administered for 20 minutes, and then the cornea is exposed to 30 minutes of UV light. Then a contact lens is placed on the eye for comfort. In both techniques, you will be given eye drops to reduce discomfort and an antibiotic eye drop.
You eye is given numbing eye drops and you are awake. You will feel slight discomfort from the eyelid holder which helps to keep your eye open. There is also some discomfort associated with staring at a bright light.
Most people can go back to work the next day after epi-on and in 1-2 days after epi-off.
Dr. Levinson will discuss the pros and cons of both techniques, and you will be given a choice.
At this time, no insurance carriers are covering collagen cross linking. You can use Flex spending accounts, and we do offer financing for the procedure. Please ask us about these options.
